The following to just part of a longer report by the Physicians for a National Health Program on Medicare Advantage healthcare programs offered by commercial entities. It lays the foundation as to why Medicare Advantage is more expensive than Traditional Medicare. I will do doing the other parts to this report over the next few days.
MA Overpayment Report
“Our Payments and Their Profits”
As an example of the cost of Medicare Advantage . . . By an estimate and based on 2022 spending, Medicare Advantage overcharges taxpayers by a minimum of 22% or $88 billion per year, and potentially by up to 35% or $140 billion. By comparison, Part B premiums in 2022 totaled approximately $131 billion, and overall federal spending on Part D drug benefits an approximate $126 billion. Either of these or other crucial aspects of Medicare and Medicaid. could be funded entirely by eliminating overcharges in the Medicare Advantage program.
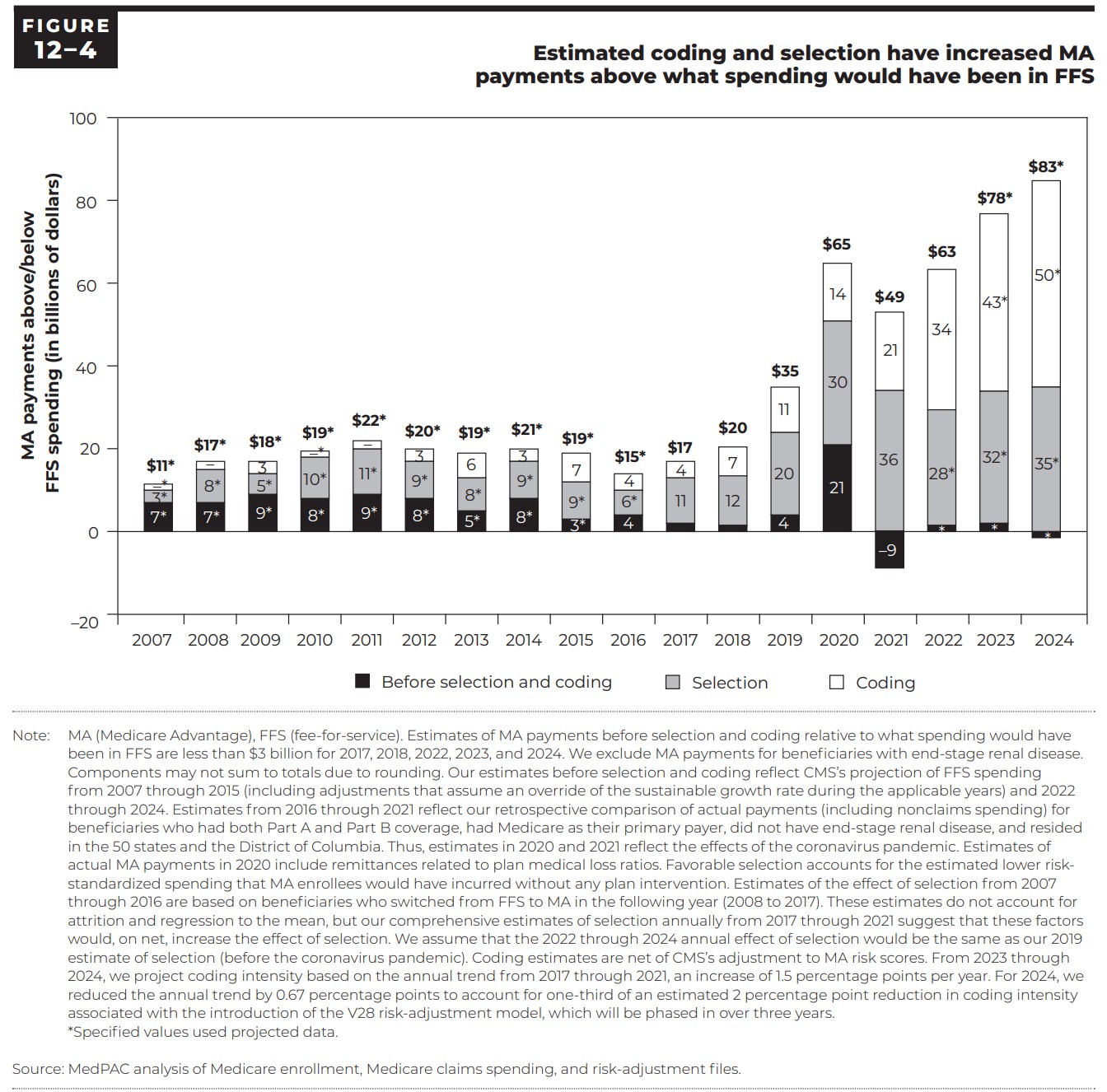
The assumption is the Medicare Advantage overcharges are greater than the $83 billion as depicted in Chart 12-4, page 377 of The Medicare Advantage program: Status report by Medpac.
Managed care proponents have maintained programs like MA reduce expenditures, improve quality of care, and enable consumer choice. The reality is just the opposite. The data shows privatized Medicare has not once yielded savings for the program.
Conservative estimates by the Medicare Payment Advisory Commission (MedPAC) show the payments to MA plans over the past two decades have always been higher than they would have been for patients in Traditional Medicare. Despite the additional spending, MedPAC could not say conclusively whether care outcomes fared better under MA. Patients in Traditional Medicare have access to nearly all doctors and hospitals across the country. While those in MA must contend with limited networks and prior authorization procedures limiting the “choices” consumers are able to make.
All of these are serious issues. This report deals with the first problem: “overcharging in Medicare Advantage.” Various elements of MA by design or by consequence, result in a much higher level of government spending than is necessary to provide Medicare benefits. The money goes to corporate profits. Instead of creating a more efficient system of care, large corporations are using MA as their cash cow, taking billions in taxpayer dollars while using delay or deny tactics in the treatment of Medicare patients.
Favorable Selection
Payments to MA plans rely on comparisons made to beneficiaries in Traditional Medicare. In this system, Medicare sets a “benchmark,” representing a certain percentage of the average level of spending for a beneficiary in Traditional Medicare within a given county. The benchmark can vary from 95% of the average in counties with the highest spending, to 115% in counties with the lowest spending.
MA plans submit a “bid” representing their estimation of total costs to cover all Medicare benefits for an average beneficiary in the county. (7) This includes money allocated to administrative overhead and profit for the insurer. These bids are multiplied by a risk adjustment score based on a combination of demographic and diagnostic factors. If MA plans bid below the benchmark, the plan is allowed to keep approximately two-thirds of the difference, which is used to reduce cost-sharing for enrollees or improve benefits. (8)
One problem is the process assumes, after risk adjustment the average spending for patients in MA is more or less the same as average spending for patients in Traditional Medicare. However, MA plans benefit from “favorable selection.” The beneficiaries who join MA plans are generally healthier and therefore less costly.
A 2019 KFF study compared the spending levels for two groups of beneficiaries who both started in Traditional Medicare. One group stayed in the program, and the other moved to MA. Compared to the group that stayed, the group moved to MA cost on average $1,253 per year less while in Traditional Medicare or a 13% difference in spending. Even beneficiaries with chronic conditions requiring additional care, if they moved to MA, were found to have cost over $1,000 less than their counterparts who remained in Traditional Medicare. These figures were found after using a risk adjustment model very similar to Medicare’s own, making clear that the adjustment process inadequately addresses this issue. (9)
MedPAC’s June 2023 report to Congress estimated favorable selection across the entire MA population resulted in a level of spending approximately 11% lower than for Traditional Medicare beneficiaries with the same risk score in 2019. (10) MA beneficiaries were found to have had lower levels of spending for multiple years prior to entering their MA plan. The effects of favorable selection persisted for years after they joined. (11) Another study by the USC Schaeffer Center estimated overpayments from favorable selection to be even higher at 14%, an effect which again was apparent even after the application of risk adjustment. (12)
Several factors potentially contribute to this phenomenon. Patients who are sicker have more complicate care needs may be turned off by limited networks of MA, the use of prior authorizations, and other care denial strategies in MA plans. (13) By contrast, healthier patients may feel less concerned about restrictions on care and more attracted to common features of MA plans like $0 premiums and additional benefits (e.g. dental and vision coverage gym memberships, etc.).
Insurers can use strategies such as targeting advertisements reaching out to the patients most favorable to their profit margins. Risk adjustment in MA as it stands is not capable of fixing these issues. One study published in the American Economic Review suggests insurers respond to risk adjustment simply by switching from seeking out the cheapest patients overall to seeking out the cheapest patients who have conditions included in the adjustment model. (14)
The problem? MA plans are paid as though their enrollees have the same health needs and require the same levels of spending as their Traditional Medicare counterparts. As detailed, this is untrue. The health difference between the two groups results in overpayment to Medicare Advantage plans which favor healthier insures. The difference in payment is anywhere from 11-14%, or about $44-56 billion per year based on total MA spending for 2022.
See MA Overpayment Report for corresponding footnotes.
There is evidence that besides healthier and less costly individuals moving into MA, less healthy and more costly individuals are moving out of MA. We could term this “favorable deselection,” which would have the same type of effect on payments.
A 2019 study in JAMA Internal Medicine found that both high-need patients (those with several chronic conditions) as well as dual-eligible patients (those who qualify for both Medicare and Medicaid due to lower income) switched from MA to Traditional Medicare at higher rates compared to other patients. (15) These findings were echoed in an earlier study conducted in 2015, which found that patients in high-cost services like nursing homes and home health care tended to switch from MA to Traditional Medicare at higher rates than the reverse. (16).
See MA Overpayment Report for corresponding footnotes.
Ending Overpayment in Medicare Advantage – Center for American Progress
Medicare Advantage Plans’ Prior Auth Rules Would Be Made Public Under CMS Proposal | MedPage Today